Most psychiatric disorders are still diagnosed purely based on observed behaviour. Unlike other medical fields, such as oncology, psychiatry lacks biological tools to support diagnosis, stratification, or treatment selection. For neurodevelopmental disorders, this limitation is especially problematic. Conditions like autism spectrum disorder (ASD) and schizophrenia begin early in life, evolve differently across individuals, and respond inconsistently to treatment. These features make them strong test cases for developing biomarker-based precision medicine.
Using biomarkers in neuroscience, i.e. using biological indicators of normal or pathological processes, holds promise for enhancing the detection and management of such disorders. Yet, despite decades of research, few discoveries have been translated into clinical use. This post explores the current landscape of biomarkers in ASD and schizophrenia.
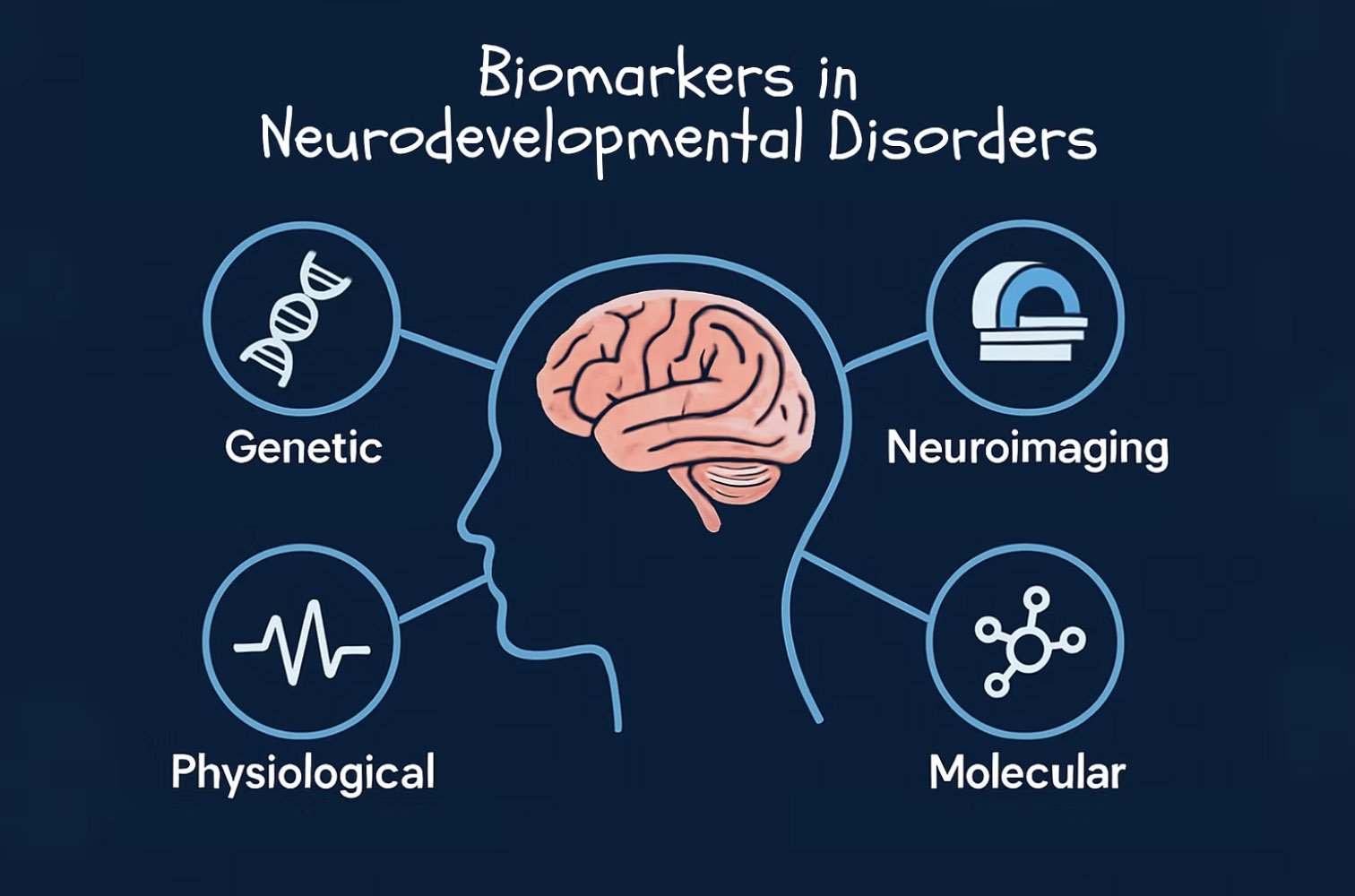
Biomarkers can be genetic, molecular, physiological, or neuroimaging-based indicators of health or disease, and are typically grouped by their intended function: diagnosing disease, predicting progression, monitoring treatment response, or assessing risk. The FDA–NIH BEST framework outlines seven such categories, from risk markers to safety biomarkers for adverse drug effects¹.
In psychiatry, the BEST categories help clarify how biomarkers might support not just diagnosis, but also patient stratification and treatment guidance. Importantly, they offer a foundation for more objective, reproducible decision-making in a field long dominated by subjective criteria.
Improving outcomes in neurodevelopmental disorders like ASD and schizophrenia depends not just on early identification, but on accurately capturing individual differences. Both disorders are biologically heterogeneous, meaning that similar symptoms can arise from different underlying mechanisms. Biomarkers offer a way to move beyond these broad diagnostic categories by identifying biologically distinct subgroups that may respond differently to treatment.
In ASD, biomarkers currently explored are primarily genetic or immune-based risk indicators. For example, rare copy number variants, de novo mutations, and altered microRNA profiles have all been associated with increased risk of disease onset²⁻⁴. Environmental factors, such as maternal immune activation during pregnancy, also contribute to risk. For instance, elevated levels of IL-6 or TNF-α in pregnant mothers have been linked to autism-like outcomes in offspring⁵⁻⁶. Still, no individual biomarker, or combination of markers, has reached sufficient predictive accuracy for clinical application.
Some stratification efforts already show promise. A longitudinal study found that increased extra-axial cerebrospinal fluid at 6 months of age predicted ASD diagnosis with 69% accuracy⁷. Similarly, fMRI studies consistently show that early speech-related hypoactivation can predict more severe language deficits later⁸. These examples illustrate how risk and prognostic biomarkers can overlap, identifying both who is likely to develop a disorder and how it may progress.
Schizophrenia has a longer track record in biomarker research. Structural abnormalities, such as hippocampal volume loss and reduced cortical thickness, as well as neurochemical disruptions in dopamine and glutamate signalling, are among the most consistently reported findings⁹⁻¹⁰. While these markers lack diagnostic specificity, they have proven more useful in predicting outcomes and guiding treatment. For instance, reduced P300 amplitudes in EEG recordings may indicate how well a patient will respond to therapy¹¹. Similarly, grey matter reductions and distinct glutamatergic profiles have been linked to long-term functional outcomes¹²⁻¹³. These advances have led to emerging 'biotype' classifications, grouping patients by biological characteristics rather than symptoms¹⁴.
While biomarkers for diagnosis are still in early development, those that guide treatment may be easier to identify as they respond to specific interventions. But here, too, progress has stagnated.
In ASD, there are currently no pharmacological treatments for core symptoms, such as social deficits and repetitive behaviours. Instead, medications like SSRIs and antipsychotics are sometimes used to manage secondary symptoms, like hyperactivity and irritability. Biomarkers such as EEG changes and shifts in serotonin levels have been explored to track treatment effects¹⁵⁻¹⁶, but the heterogeneity of ASD makes it difficult to identify consistent, reliable targets. Additionally, because ASD is not a degenerative condition, biomarkers for monitoring disease progression are limited and less commonly used.
By contrast, schizophrenia treatments, especially antipsychotic medications, have clearer biological targets. PET scans have been used to optimise D2 receptor occupancy and reduce its side effects¹⁷. Blood-based cytokines, like IL-6 or IL-1β, are being explored to track treatment response and inflammation¹⁸. Pharmacogenomics also plays a role: liver enzyme genotyping may explain variability in drug metabolism and inform personalised dosing¹⁹. Despite these developments, no biomarker has yet become a routine part of schizophrenia care. Most remain in the experimental or research phases.
Several challenges prevent biomarker translation into clinical psychiatry:
To address these issues, researchers advocate for large, longitudinal, multicenter studies with standardised methods. Projects like LEAP (Longitudinal European Autism Project) aim to validate stratification biomarkers in ASD²³. Others promote open science, multimodal markers, and transdiagnostic frameworks that move beyond traditional categories²⁴.
Biomarkers offer an opportunity to ground psychiatric diagnosis and treatment in biology, bringing much-needed precision to fields like neurodevelopmental disorders. While significant hurdles remain, ongoing efforts in standardisation, replication, and integrative biomarker development hold promise. The goal is not to replace clinical observation but to enhance it by guiding interventions that are timely, tailored, and evidence-based.